Genetics: the misconceived link between autoimmune disease and depression
Some genes responsible for autoimmune diseases do not explain the depression that affects a large number of patients, according to a large study conducted on more than 130,000 people.
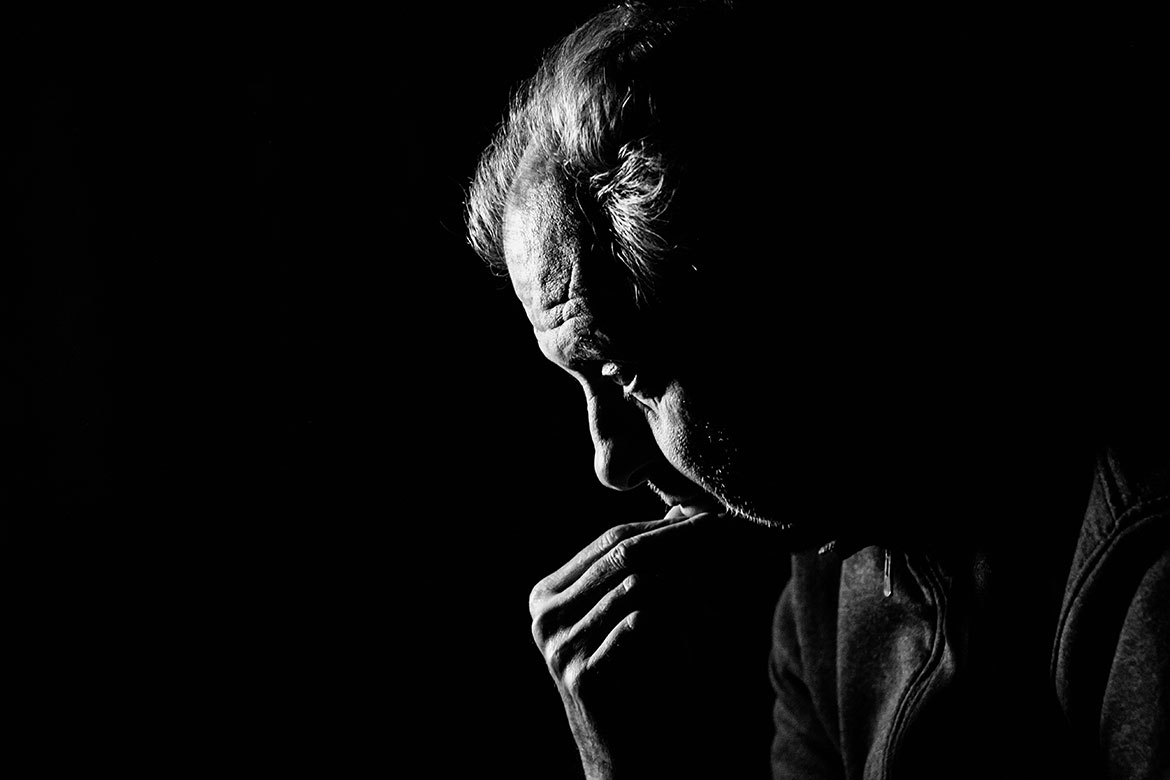
Depression and autoimmune diseases often occur together, but there is no genetic proof of any connection. | Image: shutterstock/Andrew Stripes
There is a higher rate of depression in patients with autoimmune disease, i.e., illness due to abnormal reactions of the immune system. This happens when the disease is linked to a genetic predisposition, e.g., multiple sclerosis, psoriasis, Crohn’s disease or type 1 diabetes. An international consortium has now analysed whether the genes associated with the development of autoimmune disease are correlated with an increased risk of depression. Geneticists have studied the so-called HLA system, located on Chromosome 6, and in particular a sub-set where there’s an established association between autoimmune diseases and schizophrenia.
The consortium analysed these genetic variants in 45,149 people with depression and 86,698 healthy individuals (control group). The Lausanne University Hospital (CHUV) contributed data from 1,500 patients and 2,000 control subjects. The results show that the risk of depression was not increased by any variant of HLA genes playing a major role in the genetic susceptibility of autoimmune diseases or associated with the risk of schizophrenia. There does not, therefore, appear to be a genetic factor common to depression and autoimmune diseases within the HLA system.
“There must consequently be other genes or biological mechanisms, outside the HLA system, that can explain the link between depression and autoimmune disease observed epidemiologically”, says Martin Preisig, a CHUV researcher and co-author of the study. “It should be kept in mind, however, that depression is a very diverse disorder and that it is always possible for HLA gene variants to be associated with some subgroups of depressive disorder, but not with depression across the board”.