Sleeping bacteria evade antibiotics
Besides building up resistance, bacteria have another means of protecting themselves against antibiotics. But it’s quite possible that too little attention has been paid to it in the clinical environment.
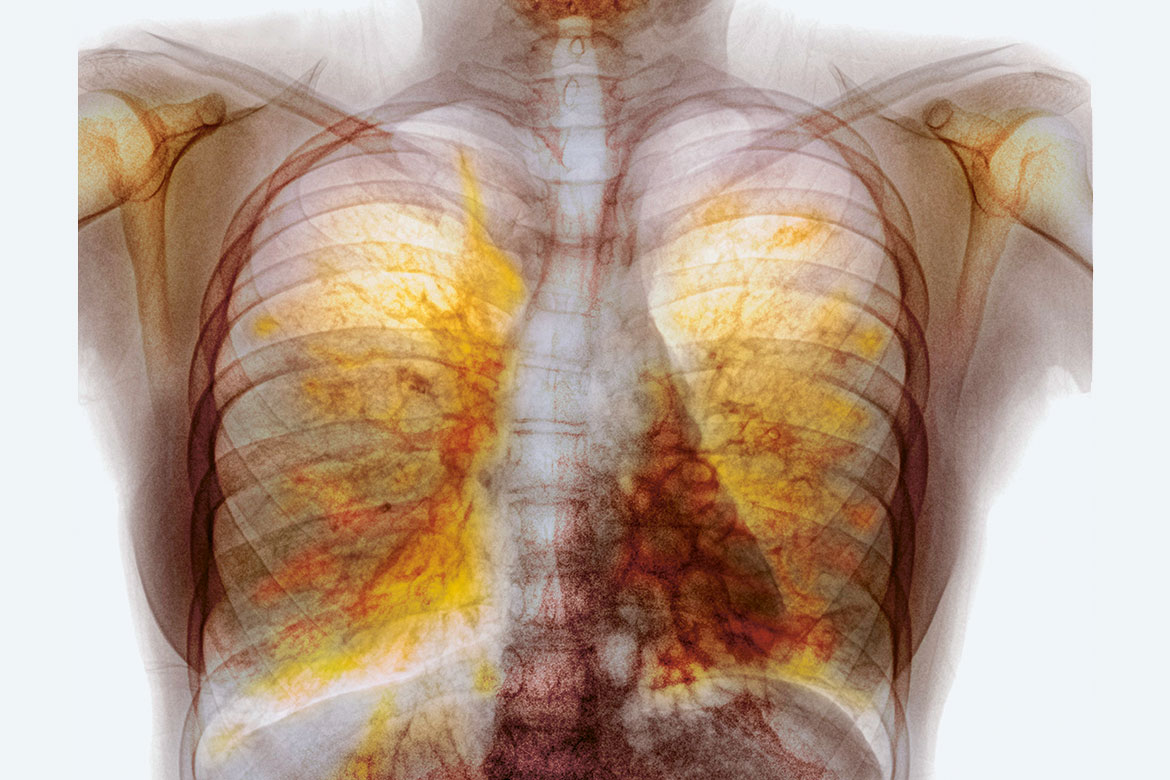
In the lungs of a patient with cystic fibrosis, germs can lead to chronic inflammation because they go into hibernation to evade antibiotics. | Image: Keystone/Science Photo Library/Photostock-Israel
Increasingly, bacterial pathogens are developing resistance to specific active agents by means of genetic adaptation. But there is another way in which bacteria can evade treatment by antibiotics – by going into a kind of deep sleep. Many of the usual antibiotics disturb important metabolic processes during cell reproduction, so for them to work, the bacteria have to be active and multiplying. If the bacteria are in ‘hibernation’, however, most antibiotics are unable to do anything to them.
Bacteria that survive in this way are called antibiotic tolerant. Whereas resistant pathogens are all equally immune to certain antibiotics, it is often just a small proportion of tolerant bacteria that fall into a deep sleep; the others die when the drug is administered.
Reasons for therapy failure
But these less robust sleepers that are expressly tolerant – so-called persisters – are important to clinicians. “They might be responsible for many chronic infections that keep returning, time and again, even though the antibiotics are actually working”, says Annelies Zinkernagel of the Department of Infectious Diseases and Hospital Epidemiology at the Zurich University Hospital. This kind of persistence is especially prevalent in cases of infection that begin with biofilms on prostheses.
This phenomenon has been known about since the 1940s, but it has only been possible to investigate it precisely in the past few years. This is because microbiological methods are designed to characterise the growth of organisms – and persisters are notable for their absence of growth. But now Zinkernagel and her team have proven for the first time in two studies that persistence was the reason for failed treatments, not resistance. Both patients in question suffered from an abscess or infection in a heart pacemaker that was triggered by a staphylococcus infection. In the second case, the implant ultimately had to be replaced.
Harbingers of resistance
“We were able to observe an increase in persisters during the antibiotic treatment”, said Zinkernagel, “and we discovered that certain persistent pathogens also develop resistance over time”. Persistence could thus be significant in clinical practice, both on its own accord and with regard to the formation of resistance. This is also the conclusion of Urs Jenal of the Biozentrum of the University of Basel. He is investigating the pseudomonas bacteria in patients with cystic fibrosis who suffer from chronic lung infections. Samples from the Basel University Hospital show that specific germs in the lungs developed persistence, but no resistance, even after long-lasting, repeated treatment with antibiotics. Other germs from the lungs of the same patients, however, show increasing resistance.
“We believe that moderate antibiotic tolerance is a precursor of both resistance and of pronounced persistence. Both these strategies on the part of the bacteria can provide them with advantages during a treatment”, says Jenal. What’s more, lab experiments suggest that antibiotic treatment can quickly lead to tolerance and that this in turn can accelerate the development of resistance. “Employing two different antibiotics at the same time can prevent the formation of resistance”, says Jenal, “but tolerance and increased persistence will develop nevertheless”.
So it is all the more important to explain the mechanisms that bacteria use to enter into their deep sleep. This could provide new approaches to identifying the pathogens in question and to attacking them with innovative agents, despite their being dormant. Or perhaps one might target them so as to waken them – and thereby make them vulnerable to today’s existing antibiotics.