The complicated hunt for personalised data
Everyone dreams of bespoke therapies for each individual patient. But one biostatistician claims that conventional clinical studies aren’t providing the necessary data.

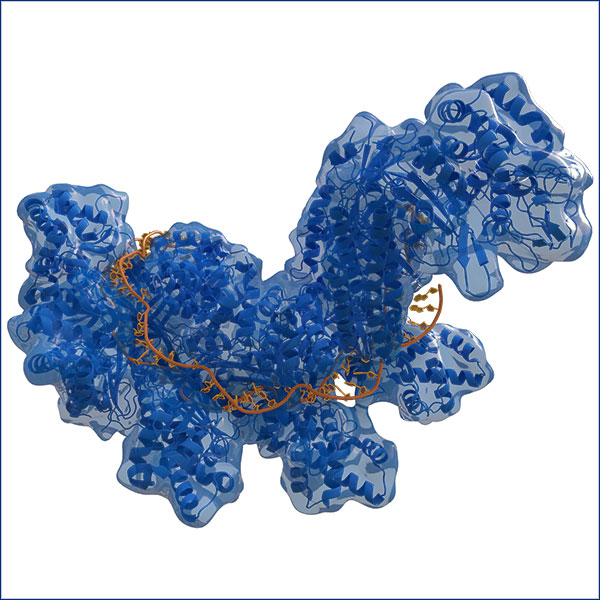
Personalised medicine aims to provide bespoke therapy, but research struggles to distinguish differences among patients and natural individual variations. | Photo: Viacheslav Lopatin/Shutterstock
Medicine has a problem. Usually, only a certain number of patients will respond to a therapy. For example, according to the US Food and Drug Administration (FDA), anti-depressants are ineffective in 40 percent of those treated with them. The reason for this is believed to lie mostly in our genes.
It is these differences between patients that provide the starting point for personalised medicine. One example is the cancer drug Iressa. It will only work with patients whose tumour cells reveal mutations in a specific gene – it is a growth factor that stimulates cell division. These mutations are a so-called ‘biomarker’ that indicates whether or not a patient will respond to the therapy.
Trying to determine the differences between patients is far more difficult than you might think. This is the opinion of Stephen Senn from the Luxembourg Institute of Health. “In a clinical study, it’s normally impossible to determine who has benefitted from the treatment and who hasn’t”, says Senn. “The hype around personalised medicine is based on a hypothesis that’s barely been tested, namely that patients’ reactions to a therapy vary greatly”. Senn believes that claims about responders and non-responders such as are quoted by the FDA are in fact based on shaky statistical foundations.
This is because the studies don’t compare the reactions of individual patients. Instead, whole groups of patients are compared with control groups on the basis of average responses – such as the difference in the blood pressure of all the patients who have received a therapy compared to those who were given a placebo. “Quite simply, we’re not carrying out the type of studies that would enable us to differentiate responders from non-responders”.
Senn does not deny that genetic differences among patients can have an impact on the success of a therapy. He’s saying that most clinical studies are not in a position to decide whether there are genetic origins behind the different therapeutic results. They could also be caused by chance differences in the patients’ diet or by a hidden infection in a patient.
First the placebo, then the active substance
As a way out, Senn proposes observing patients on an individual basis over a longer space of time. They should first be given an active substance, then a placebo (or vice versa). Such so-called serial n-of-1 trials would provide data to help determine if patients’ different reactions are in fact caused by other, chance variations in the results measured. In the specialist journal Nature in 2015, Nicholas J. Schork, the director of the human biology department at the J. Craig Venter Institute in La Jolla, California, observed that “Researchers need to probe the myriad factors – genetic and environmental, among others – that shape a person’s response to a particular treatment”.
Such n-of-1 trials are also controversial. Peter Jüni is a Swiss epidemiologist and the Director of the Applied Health Research Centre at the University of Toronto. He does not think that n-of-1 trials are really practicable, because they are too protracted and too complicated for clinics to carry out. He agrees with Senn that studies are providing too many unfounded conclusions about responders and non-responders. Nevertheless, if you proceed in a “highly disciplined” manner, he says, there are still ways in which you can interpret traditional studies correctly.
However, you have to be aware that results from specific patient subgroups are often over-interpreted. “There’s still no such thing as a truly personalised medicine in which every patient gets the exactly appropriate therapy”, says Jüni. “We can’t fulfil these expectations as of yet”. This is why efforts to provide a better data foundation for personalised medicine are important, even if Senn’s provocative ideas are disputed among experts.
Sascha Karberg is the science editor at the Tagesspiegel in Berlin.